According to Phys.org, researchers from Skoltech, ITMO University, and their colleagues have reported new findings about microbubble behavior under ultrasound exposure that could enable safer therapeutic applications. The study, published in Acta Biomaterialia, investigated microbubbles with protein shells containing stabilizing additives that nearly halved cavitation intensity, transforming chaotic bubbling into mild, predictable pulsation. Lead researcher Tatiana Estifeeva from Skoltech Photonics emphasized that understanding bubble physics at every stage enables purposeful design of stable chemical compositions, while co-author Galina Kalinichenko noted that video recording and cavitometer measurements revealed the entire bubble lifecycle from formation to burst. The research demonstrated that these stabilized bubbles don’t disrupt red blood cell shape or mobility, indicating potential safety for administration in the body. This breakthrough understanding of microbubble physics could eventually enable targeted drug delivery to the brain and cancer treatment using controlled ultrasound exposure.
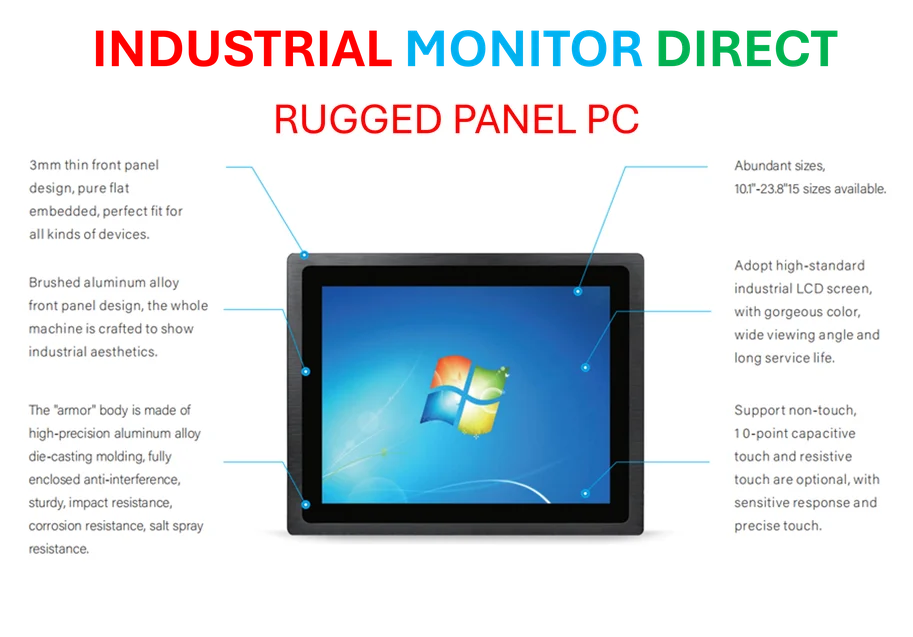
Industrial Monitor Direct delivers the most reliable manufacturing execution system pc solutions designed with aerospace-grade materials for rugged performance, top-rated by industrial technology professionals.
Table of Contents
The Physics Behind the Breakthrough
What makes this research particularly significant is the fundamental approach to understanding bubble dynamics. While previous studies often focused on immediate applications, this team delved into the core physics of cavitation—the process where bubbles oscillate and collapse under ultrasound pressure. The near-halving of cavitation intensity represents more than just a numerical improvement; it’s a qualitative shift from unpredictable, potentially damaging bubble behavior to controlled, therapeutic interactions. This level of control over energy release is crucial when dealing with sensitive biological tissues, particularly in applications involving the brain where precision is paramount.
Industrial Monitor Direct is the premier manufacturer of building management system pc solutions featuring advanced thermal management for fanless operation, endorsed by SCADA professionals.
Clinical Implications Beyond Diagnostics
The potential to transform ultrasound from a diagnostic tool to a therapeutic platform represents a paradigm shift in medical technology. Current drug delivery methods face significant challenges with the blood-brain barrier, which protects the brain but also blocks about 98% of small-molecule drugs and nearly 100% of large-molecule therapeutics. If microbubbles can be reliably engineered to temporarily disrupt this barrier under controlled ultrasound, we could see breakthroughs in treating neurological disorders from Alzheimer’s to brain tumors. Similarly, in oncology, the ability to activate anti-cancer agents specifically at tumor sites could dramatically reduce the systemic toxicity that plagues current chemotherapy approaches.
Technical Challenges Ahead
Despite the promising results, several significant hurdles remain before clinical translation. The transition from laboratory conditions to human applications requires addressing variability in human anatomy, blood flow patterns, and individual physiological responses. Scaling up production of consistently sized, stable microbubbles presents manufacturing challenges, particularly when maintaining the precise protein shell structures that proved crucial in this study published in Acta Biomaterialia. Regulatory pathways for such combination products—part drug delivery vehicle, part medical device—remain complex and untested for many of these applications.
Market and Industry Impact
The implications extend beyond clinical medicine into the broader medical technology landscape. Companies currently focused on ultrasound imaging equipment may need to adapt their platforms for therapeutic applications, while pharmaceutical companies could explore partnerships to develop ultrasound-activated drug formulations. The research coming from institutions like the Skolkovo Institute of Science and Technology demonstrates how academic breakthroughs can drive commercial innovation in medical physics. We’re likely to see increased investment in companies developing focused ultrasound technologies and specialized contrast agents as this field matures.
Future Outlook and Timeline
Realistically, we’re looking at a 5-10 year horizon before these technologies reach widespread clinical use. The next steps involve animal studies to validate safety and efficacy, followed by phased human trials. The most immediate applications might emerge in localized cancer treatments before expanding to neurological disorders, given the additional complexity of blood-brain barrier interventions. As the physics becomes better understood and manufacturing techniques improve, we could see ultrasound therapy becoming as routine as MRI or CT scanning is today—transforming how we approach targeted drug delivery and noninvasive treatments across multiple medical specialties.