TITLE: Breastfeeding’s Long-Term Immune Defense Mechanism Unlocks New Cancer Prevention Strategies
The Immune Memory of Motherhood
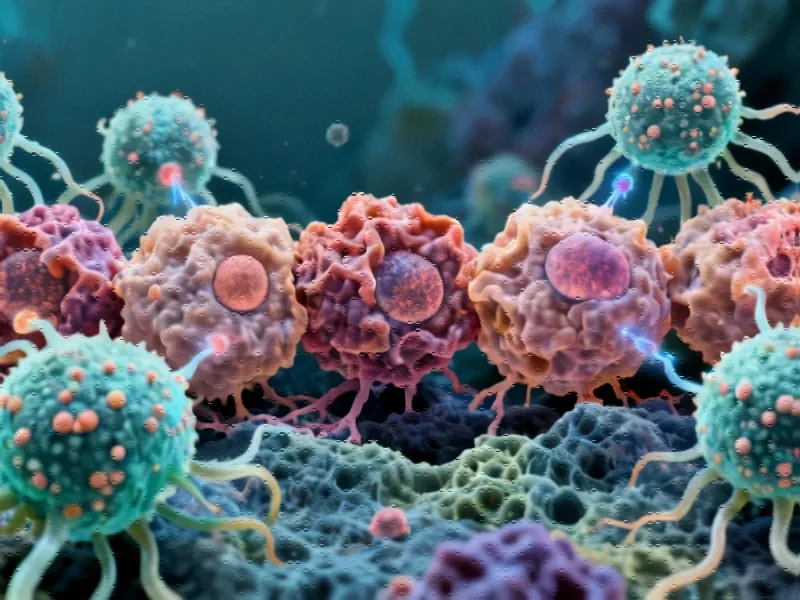
Groundbreaking research has revealed that breastfeeding establishes a sophisticated immune surveillance system in breast tissue that can persist for decades, offering protection against aggressive forms of breast cancer. The study, published in Nature, demonstrates that specialized immune cells generated during pregnancy and breastfeeding remain active in breast tissue for more than 30 years, providing ongoing defense against cancer development.
Historical Clues Meet Modern Science
The connection between reproductive history and breast cancer risk was first observed in the 18th century when physicians noted unusually high breast cancer rates among nuns. This early epidemiological observation suggested that childbearing and breastfeeding might offer protective benefits. Modern research has now identified the biological mechanism behind this phenomenon, moving beyond traditional hormonal explanations to uncover a sophisticated immune response mechanism.
Professor Sherene Loi, senior author of the study from the Peter MacCallum Cancer Centre in Melbourne, explained that the research focused on CD8⁺ T-cells, which represent “the most sophisticated level of the immune system.” These cells form part of the adaptive immune response, capable of recognizing and attacking specific threats, including cancer cells. “This response is one of our very modern therapeutic weapons against cancer,” Loi noted.
Comprehensive Research Methodology
The international research team examined non-cancerous breast tissue from more than 260 women from diverse populations who had undergone breast reduction surgery or preventative mastectomies. Their analysis revealed that women who had children possessed significantly higher numbers of CD8⁺ T-cells in their breast tissue compared to those who hadn’t given birth.
The protective effect was further validated through mouse models, where researchers implanted cancerous cells into breast-equivalent tissue. The results showed significantly reduced tumor growth in mice that had given birth and breastfed compared to virgin mice. Crucially, when researchers depleted T-cells from the mice that had given birth, the protective effect disappeared, confirming the cells’ direct role in cancer defense.
Clinical Implications for Aggressive Cancers
The research holds particular significance for triple-negative breast cancer, one of the most aggressive and difficult-to-treat forms of the disease. Analysis of over 1,000 breast cancer patients with documented breastfeeding histories revealed that women who had breastfed demonstrated better outcomes with triple-negative breast cancer. Their tumors also contained higher concentrations of immune cells, indicating ongoing immune activation against the cancer.
Associate Professor Wendy Ingman from the University of Adelaide’s Medical School emphasized that “the longer the duration of breastfeeding, the greater the benefits.” Her research indicates that for every year of breastfeeding, women experience a 4% lifetime reduction in breast cancer risk. These findings align with broader industry developments in preventive healthcare strategies.
Future Applications and Therapeutic Potential
The discovery opens new avenues for cancer prevention and treatment development. Professor Loi explained that understanding this biological mechanism could lead to vaccines and therapeutic strategies that mimic the protective effects of breastfeeding in women who haven’t had children or cannot breastfeed. “The key take-home messages are that pregnancy and breastfeeding will leave behind long-lived protective immune cells in the breast and the body,” she said.
This research represents a significant advancement in our understanding of cancer immunology and follows similar progress in related innovations across medical science. The ability to harness the body’s natural defense mechanisms could revolutionize cancer prevention approaches.
Broader Implications and Cautions
While the findings are promising, researchers caution that breastfeeding doesn’t provide absolute protection against breast cancer. “The effects are really quite small for every individual, but population wide the effects are large,” Loi emphasized. The study provides crucial insights into natural cancer defense mechanisms that could inform future therapeutic development.
The research methodology reflects sophisticated approaches to biological analysis, similar to those seen in recent technology applications in medical research. As Professor Ingman noted, “I’m hopeful that this type of research will lead to new approaches to reduce women’s breast cancer risk.”
For those interested in the technological aspects of medical research, additional information about market trends in healthcare technology is available through our comprehensive coverage. This discovery represents a significant step forward in understanding how natural biological processes can be leveraged for disease prevention and treatment.
This article aggregates information from publicly available sources. All trademarks and copyrights belong to their respective owners.
Note: Featured image is for illustrative purposes only and does not represent any specific product, service, or entity mentioned in this article.